Analysis of Effectiveness of Online CBT Treatment for Trichotillomania
Does it Work?
If you have been struggling with trichotillomania, it could be that shame and stigma have prevented you from seeking treatment, or that you were unable to find appropriate treatment. Mental health professionals who understand the nature of the problem are rare and treatments are usually costly.
At TrichStop we have developed an online therapy program available at a fraction of the cost of traditional face-to-face therapy Our program is based on different types of CBT adjusted for online work and text-based approach. Especially if you’re not familiar with how CBT works, you may be apprehensive about the program, perhaps most of all because it’s a form therapy administered over the internet. This page will provide you with the basics of how our program works.
A psychotherapy approach called cognitive behavior therapy (CBT) is the treatment of choice for BFRBs.

What is CBT for Trichotillomania?
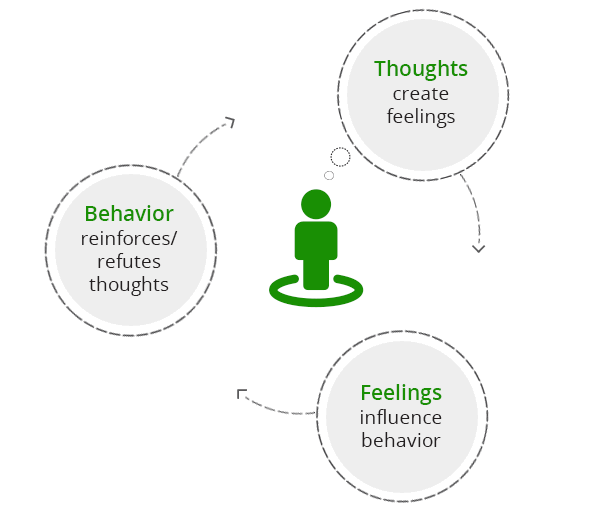
CBT or cognitive – behavioral therapy is a popular form of psychological treatment based on the idea that our psychological problems have roots in unhelpful ways of thinking, coupled with inefficient behavioral patterns. CBT therapists make an effort to help their clients become aware of these ways of thinking and the difficult feelings they cause, as well as to replace them with functional, healthier patterns. CBT is characterized by a practical, problem-solving approach.
CBT doesn’t focus on solving all your problems as much as it focuses on helping you learn how to be your own therapist, which is a highly sustainable approach to mental health issues. Unlike other schools of psychotherapy such as psychoanalysis or constructivism, CBT typically isn’t concerned with our past. It focuses more on defining what is the problems and how to go about solving it. Our therapists often have additional trainings and knowledge and if you wish to explore the “why” in addition to the “what” and the “how”, you may.
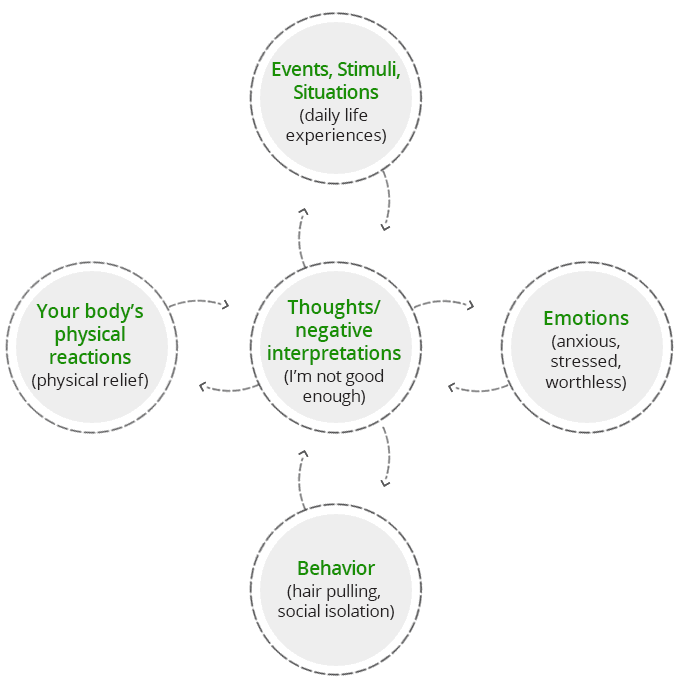
Hair pulling arises in response to negative thoughts and emotions and it provides relief from them. The relief many experience from hair pulling helps maintain the behavior regardless of its unintended effects. Hair pulling, therefore, becomes a learned response to events or situations that elicit stress or anxiety. In some cases, hair pulling can arise as a response to traumatic memories too. The goal of CBT for trichotillomania is therefore to help you unlearn the reaction of hair pulling in response to certain stimuli, and to replace it with more acceptable alternatives.
Over the years, many different forms of CBT have been developed, each emphasizing a different aspect of the cognitive – behavioral sequence (Figure 1), and addresses the hair pulling cycle (Figure 2) from a different point, using different tools. In order to provide comprehensive treatment to our clients, we have combined two evidence-based approaches to treating hair pulling:
- Habit reversal training
- Acceptance and commitment therapy.
Habit Reversal Training
TrichStop’s treatment protocol starts with a simple, yet effective behavioral intervention called habit reversal training – HRT. This form of treatment for hair pulling focuses on understanding the mechanics of the process, on identifying triggering events, thoughts or feelings, and then finding substitute behaviors in the form of competing responses. Competing responses help you minimize damage and take control of your behavior.
HRT is a practical, down-to-Earth approach that’s focused on breaking the habitual cycle that maintains hair pulling, but it doesn’t address thoughts and feelings related to it. Once you complete the HRT part of the program, you can expect to have better control over you behavior and to reduce hair pulling.
Acceptance and Commitment Therapy
Once you complete HRT, you slowly move on to another form of treatment based on acceptance and commitment therapy – ACT. In the first part, HRT helped you take control of pulling and gave you the option to choose healthier behavior when the urge to pull arises. ACT will help you deal with the urge itself.
ACT is a part of what is known as the third wave of CBT. That means that in addition to standard CBT features described in the beginning of the page, ACT implements other tools as well. Some of the tools that you will learn how to use include acceptance, mindfulness, cognitive defusion, as well as behavioral commitment that stems from your values.
In this type of CBT we look at hair pulling as a form of experiential avoidance, a mechanism employed to avoid intense and difficult emotional experience. Succinctly put, hair pulling comes about as a way to cope with but not fully process those difficult experiences. From the ACT point of view treatment consists in learning a different approach to our own experience, one of acceptance, mindfulness and detachment that allows us to be with our feelings but not get overwhelmed by them.
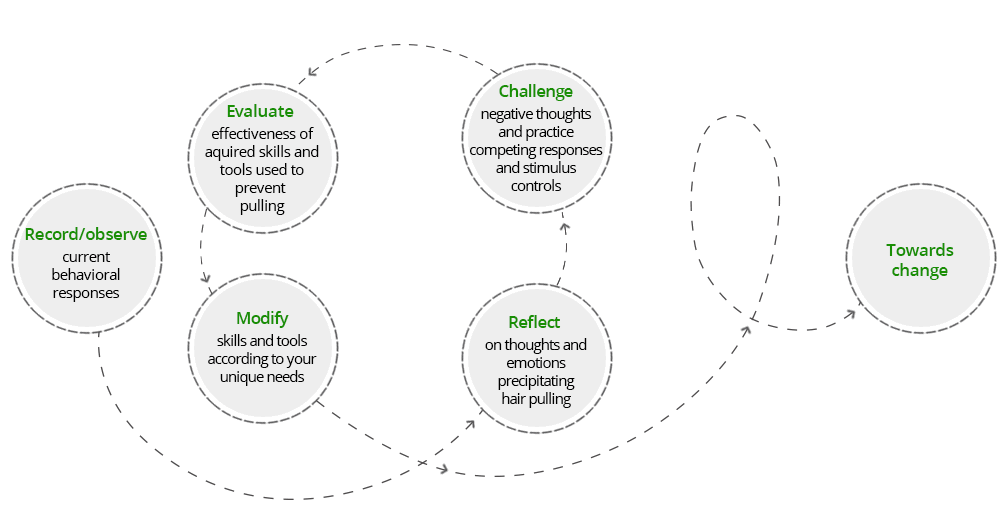
CBT differs from other therapies in that it has a clear structure and is focussed on what you are experiencing in the present as opposed to exploring events of the past. You and your therapist will work as a team to identify goals and find practical solutions to achieving them. A large component of this is reflecting on your values and vision for your life and finding ways to engage in behavior that are congruent with these.
Does CBT work for trichotillomania?
CBT is recognized among health professionals as the most effective method of treatment for body-focused repetitive behaviors such as trichotillomania. Even though medication is prescribed for the treatment of trichotillomania, FDA hasn’t approved a specific drug to treat it, and therapy remains the recommended treatment modality. One small study demonstrated the superiority of psychotherapy over medical treatment, although more research is needed to make a definitive conclusion.
Habit Reversal Training
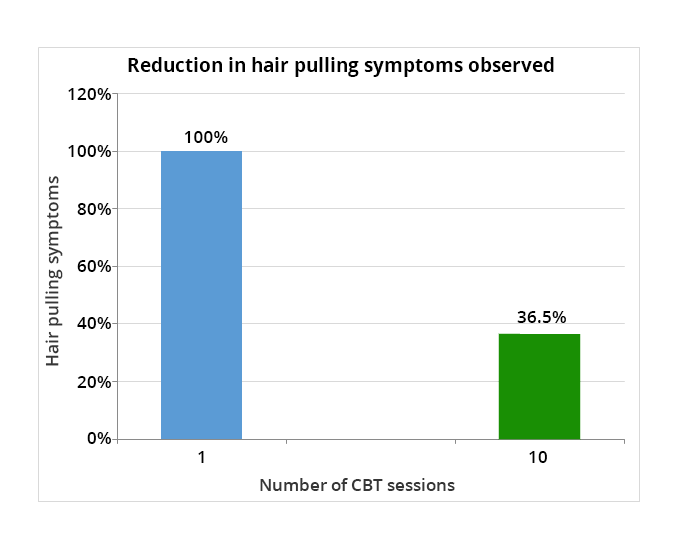
Habit reversal training is the first behavioral intervention shown to be effective for hair pulling. It was developed four decades ago as a specific treatment and has since been shown to be a highly effective intervention ever since, remaining to this day the intervention with most evidence to back up its claims of efficiency. Different studies emphasize the need for different length of treatment, ranging from 4 weekly sessions up to 22. In fact, whether it’s studied as a stand-alone treatment or in combination with ACT or DBT, habit reversal is the most tested behavioral intervention for trichotillomania. One study looking at the effectiveness of ACT and HRT found that there was a significant reduction in hair pulling severity, impairment ratings, and hairs pulled, in the participants who received ACT/HRT compared to those who were in the control group. Another study examined the efficacy of CBT and the serotonin reuptake inhibitor, clomipramine, compared with placebo in the treatment of trichotillomania. The results indicated that CBT had a dramatic effect in reducing symptoms of trichotillomania and was significantly more effective than clomipramine or placebo.
Acceptance and Commitment Therapy
Research has shown that although HRT is effective in reducing hair pulling, clients often experience relapse because HRT doesn’t seem to address all the relevant factors that lead to and maintain trichotillomania.
Acceptance and commitment therapy addresses avoidant tendencies that clients with trichotillomania exhibit, as well as its emotional dysregulation aspects, which lead to lower quality of life overall. In addition, avoidant tendencies that researchers have identified seem to produce urges of higher intensity and clients with avoidant tendencies overall have symptoms of higher intensity. In a trial of 10 ACT sessions spread over 12 weeks, researchers found that the therapy resulted in significant reduction of symptom severity, both from the point of view of clients and clinicians.
According to another small study, ACT when combined with HRT seems to produce better outcomes, as they provide a more comprehensive treatment, addressing both the habitual, behavioral aspect, as well as avoidant tendencies and emotional regulation.
Summary
Overall, current research appears to support the efficacy of both treatment modalities that TrichStop is based on, including the specific combination that our program uses. The limited amount of research available today, indicates that psychotherapy is a superior treatment modality over pharmacotherapy and is a standard to be used.
Does online CBT work?
As we’ve shown above, there is more than enough evidence to suggest that CBT for trichotillomania works well, but the evidence refers to traditional face-to-face therapy. Can internet-based therapy ever really be as effective? Even though different internet-based CBT intervention have been present for years now, the last few years have seen a dramatic increase in research interest in these types of interventions, as they make mental health service more readily available and certainly more affordable, in addition to bridging geographic gaps.
As in other areas of research, there aren’t enough studies available. "StopPulling" is an on-line, interactive self-help approach derived from evidence-based cognitive behavioral models of treatment for trichotillomania. Preliminary data from 265 users of the program during the first year of public availability suggested significant improvement in symptoms. Response rates were comparable to long-term follow-up after more intense cognitive behavioral treatment. A smaller study of an online self-help program that used decoupling and progressive muscle relaxation showed some benefit. Even though the study sample was rather small, this data is important for TrichStop, as progressive muscle relaxation is a part of the customized aspect of our program.
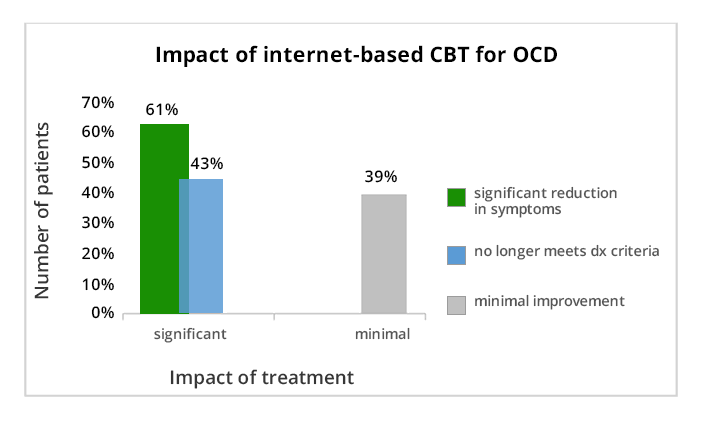
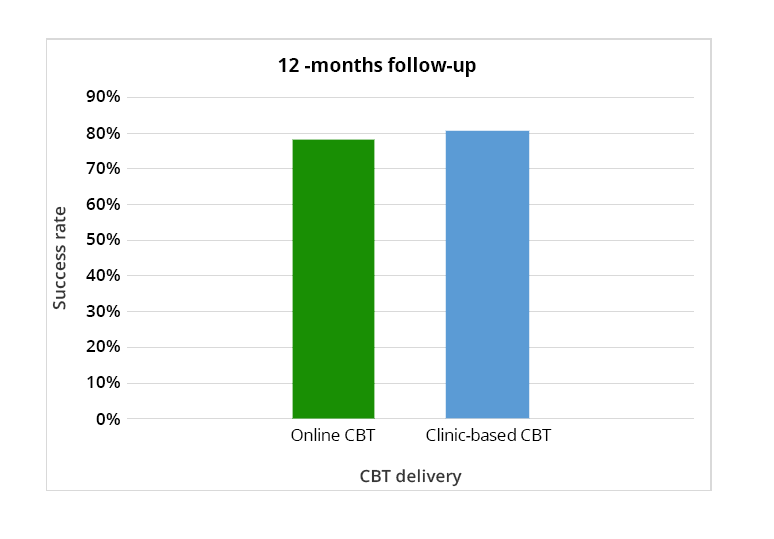
There is also evidence for the effectiveness of online CBT for other conditions such as OCD and anxiety disorders. Even though trichotillomania is a separate entity, it shares some common straits with OCD and anxiety is a commonly found symptom. This allows us to infer indirectly that such interventions may be beneficial in the case of trichotillomania too. One study that examined the relative efficacy of online versus clinic delivery of CBT in the treatment of anxiety disorders in adolescents, found that 78% of adolescents in the online group no longer met criteria for the principal anxiety diagnosis at 12-month follow-up compared with 80.6% in the clinic group.
CBT is also widely regarded as an effective treatment for obsessive compulsive disorder (OCD), but similar to trichotillomania, CBT therapists who specialize in this field are scarce. One study that evaluated internet-based CBT for OCD found that 61% of participants at post-treatment had a clinically significant improvement in OCD symptoms, and 43% no longer fulfilled the diagnostic criteria of OCD. The treatment also resulted in statistically significant improvements in self-rated OCD symptoms, general functioning and depression.